TMJ
Home | Our Procedures | TMJ
Understanding TMJ
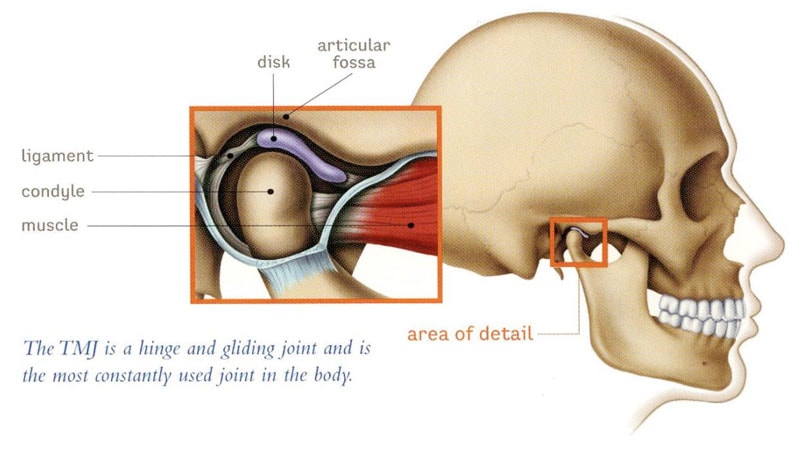
The temporomandibular joint (TMJ) is a complex structure located in front of the ear, connecting the lower jawbone (mandible) to the base of the skull (glenoid fossa). This joint enables the jaw to move smoothly when you open and close your mouth, thanks to a disc that acts as a cushion between the jawbone and the skull.
TMJ Disorders
Problems with the TMJ often occur when this cushioning disc becomes displaced. This can lead to various issues, including arthritis, which is the inflammation of the joint. Other conditions that can affect the TMJ include tumors, systemic diseases like rheumatoid arthritis, dislocations, fusion of the joint to the skull (ankylosis), abnormal growths of the jawbone (condylar hyperplasia or resorption), and trauma such as fractures near the joint. The most common sources of TMJ pain are disc disorders and arthritis.

Common TMJ Disorders
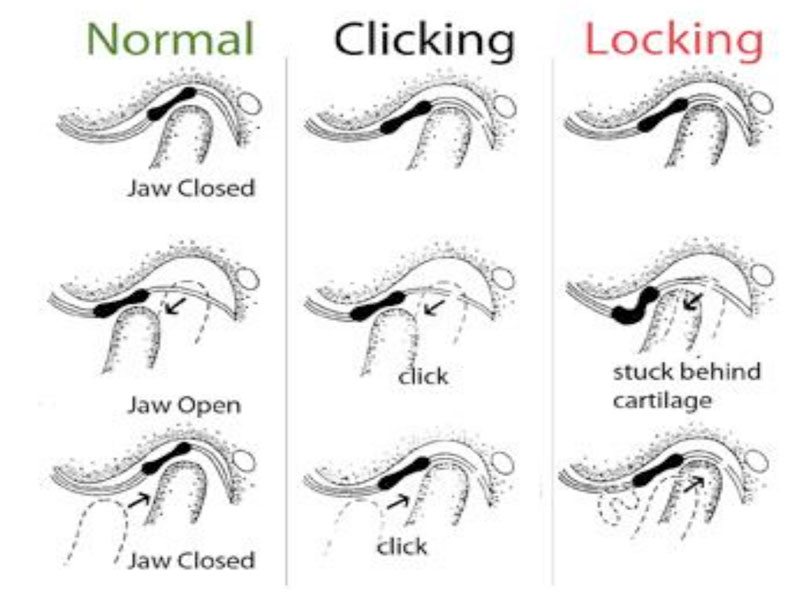
- Anterior disc dislocation with reduction- This condition occurs when the disc shifts forward from its normal position when the mouth is closed but returns to its place with a click upon opening. It often manifests as popping or clicking noises in the joint and may occasionally result in the jaw becoming temporarily stuck in an open position.
- Anterior disc dislocation without reduction- In this scenario, the disc remains displaced in front of its proper position both when the mouth is closed and as it opens. This can lead to a condition known as “closed lock,” characterized by an inability to fully open the mouth.
- Perforations of the disc- Perforations or damage to the disc can cause grating, crunching, or grinding sounds within the joint, indicating structural issues within the TMJ.
- Arthritis- Arthritis in the TMJ involves inflammation that leads to changes in the disc and bones of the joint. This inflammation often results in pain and restricted movement of the jaw.
- Chronic dislocation of the joint- Chronic dislocation refers to the joint frequently slipping out of its normal position. This ongoing instability can lead to persistent issues with jaw movement and function.
Pain stemming from the aforementioned TMJ issues can be significant. However, it’s essential to recognize that other conditions such as nighttime clenching (bruxism), muscle pain or spasms (myofascial pain), or chronic pain conditions affecting facial and neck muscles (such as fibromyalgia) can also contribute to or exacerbate joint problems. It’s crucial to address these conditions alongside TMJ issues.
Bruxism, myofascial pain, and chronic pain issues are typically nonsurgical in nature and are managed through various approaches such as medications, mouth splints, and physical therapy. At Jackson Oral Facial Surgery, we understand the complex interplay between TMJ disorders and these related conditions, and we tailor our treatment plans to address each patient’s unique needs comprehensively.
Treating TMJ Disorders
Addressing TMJ issues typically begins with conservative therapies aimed at symptom management. These may include dietary modifications to favor softer foods, applying warm compresses to the joints, and using anti-inflammatory medications like Ibuprofen or Aleve. Muscle relaxants can also be prescribed, along with methods to reduce bruxism such as medications, splints, or bite adjustments by a dentist. If these measures fail to yield improvement within 6-8 weeks, further evaluation may be necessary, often involving advanced imaging like a CT scan or MRI to assess the joint’s condition.
Surgical Treatment Options
Based on imaging findings, surgical interventions may be recommended. These can include:
-
Arthrocentesis: A procedure performed in-office under sedation to flush out the joint.
-
Arthroscopy: Inserting a small camera into the joint to assess its condition.
-
Arthroplasty: Making an incision in front of the ear to access the joint, allowing for repositioning of the disc or reshaping of the bones.
-
Modified Condylotomy: Creating a small cut in the lower jaw bone to provide space for the disc to reposition naturally. This may involve temporarily wiring the jaw shut to allow the bone to heal without altering dental alignment.
-
Orthognathic Surgery: Making small cuts in the lower (and sometimes upper) jaw bone to realign the jaws. This may require orthodontic treatment before and after surgery.
-
Total Joint Replacement: Replacing the condyle and fossa with prosthetic components, similar to knee or hip replacement surgery.
The objective of TMJ surgery is to enhance function and alleviate pain. While complete pain elimination may not always be achievable, many patients experience significant improvements in function and pain reduction, leading to a better overall quality of life.
